Interventional Cardiology
What is Interventional Cardiology?
Interventional cardiology is a highly specialized subspecialty of cardiology that focuses on the use of minimally invasive procedures to diagnose and treat heart disease. These procedures are done using small incisions and catheters inserted into the body through blood vessels.
Interventional cardiology can be used to treat a wide range of heart and vascular conditions including coronary artery disease, valvular heart disease, congenital heart disease, and peripheral arterial disease.
-
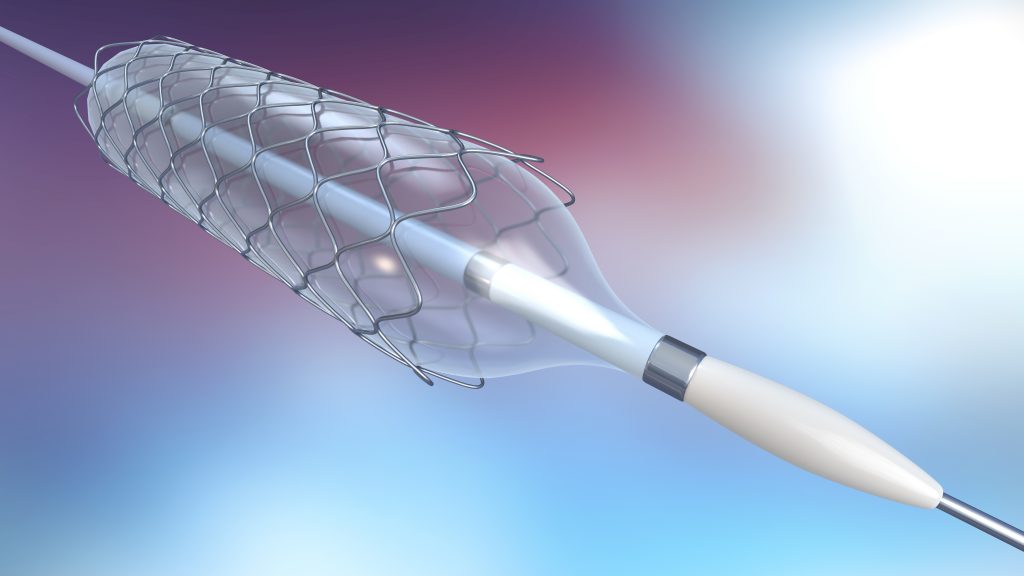
Coronary artery disease: This is a narrowing of the blood vessels that supply the heart with oxygen and nutrients. Interventional procedures such as angioplasty and stenting help to improve blood flow and reduce symptoms such as chest pain. Angioplasty and stenting are the primary methods to treat acute blockages and restore blood flow during acute heart attacks.
-
Valvular heart disease: This occurs when one or more of the heart valves does not function properly. Interventional procedures such as transcatheter aortic valve replacement (TAVR) can be used to replace the damaged valve without open-heart surgery. Novel technologies now allow treatment of additional valves, such as the mitral and tricuspid valves, without the need for open-heart surgery.
-
Congenital heart disease: These are heart abnormalities that are present at birth. Interventional procedures can be used to repair or close certain defects.
-
Peripheral arterial disease: This is a narrowing of the blood vessels that supply the legs and feet with oxygen and nutrients. Interventional procedures such as angioplasty and stenting can be used to improve blood flow and reduce symptoms such as leg pain, also known as claudication.
Interventional cardiology procedures offer several benefits over traditional open-heart surgery, including:
-
Minimally invasive: Interventional procedures are done through small incisions and catheters, which means less trauma to the body and faster recovery times.
-
Lower risk: Because interventional procedures are less invasive, there is a lower risk of complications such as infection, bleeding, and blood clots.
-
Quicker recovery: Patients who undergo interventional procedures typically have a shorter hospital stay and can return to their normal activities sooner.
Radial vs. Femoral
If you’re in need of a cardiac catheterization procedure, you may have a choice between radial catheterization (through the wrist) and femoral catheterization (through the groin). While both methods are effective, there are several benefits of radial catheterization that make it a preferred option for many patients.
-
Reduced risk of complications: One of the biggest advantages of radial catheterization is that it carries a lower risk of complications than femoral catheterization. Since the radial artery is smaller and closer to the skin’s surface than the femoral artery, it is less likely to cause significant bleeding or damage to surrounding tissues. Additionally, complications such as hematoma or pseudoaneurysm are less common with radial catheterization, which can help speed up your recovery time.
-
Improved patient comfort: Many patients find radial catheterization to be more comfortable than femoral catheterization. Since the procedure is performed through the wrist, patients are able to sit up, walk, and eat immediately. This is a particular advantage for patients with back problems because there is no need for heavy pressure on the leg and prolonged immobility.
-
Faster recovery time: Because radial catheterization is less invasive than femoral catheterization, it typically has a shorter recovery time. Patients who undergo radial catheterization can usually resume normal activities within a few hours of the procedure, whereas those who undergo femoral catheterization may need to stay in the hospital for up to 24 hours or longer and limit their physical activity for several days after the procedure.
-
Lower risk of complications, particularly in obese patients: For obese patients, radial catheterization may be a safer option than femoral catheterization. This is because the femoral artery may be harder to access in obese patients, increasing the risk of complications. Radial catheterization, on the other hand, is easier to perform in these patients and carries a lower risk of complications.
The biggest factor driving the decision to use the radial artery is the physician performing the procedure. The procedure can be more challenging technically, and the physician must have enough experience to feel comfortable with radial procedures. Many interventional cardiologists are more comfortable with the femoral approach and will therefore recommend it alone. At Ascent Cardiology, we specialize in transradial catheterization and successfully perform even the highest complexity interventional procedures through the radial approach. If you are considering a cardiac catheterization procedure, be sure to discuss your options with your healthcare provider to determine which method is right for you.